This blog is part 3 of a 3-part series transcription from a recorded webinar with Dr. Gerard Francisco of TIRR Memorial Hermann and Isha Vora, MS, OT R/L of MGH Institute of Health Professions. This webinar highlights how Paired VNS™ Therapy can help improve motor function for chronic stroke patients who have moderate to severe upper extremity impairments.
To read part 1 of this webinar transcription about chronic stroke and VNS therapy, click here.
To read part 2 about the clinical studies, click here.
The Easier Parts:
When conceptualizing the paired VNS approach, it is easy to think about it in two buckets: vagus nerve stimulation device and therapy. Even though these two parts work in great harmony to deliver the intervention, the VNS device is the easier part of this therapy to manage. The device has been FDA approved and vagus nerve stimulation has been around for about two decades for use in epilepsy or depression, so the procedure itself is familiar to neurosurgeons.
Using Vivistim in Therapy Sessions:
As a user of the of the technology during the clinical trial, I can vouch for the fact that there was a shallow learning curve in terms of implementing it. Oftentimes, implementing new technology in healthcare settings causes apprehension, however from the standpoint of using this system, it is quite easy. Over 90% of therapists said that it was not difficult to simultaneously trigger the vagus nerve stimulation while delivering the therapy.
A brief overview of what the technology entails:
- There is a laptop that communicates with a wireless trigger button the therapist controls and with the implanted device to send and trigger the stimulation.
- When the therapist presses the wireless button, you can see the user interface on the laptop that operates as a counter. This helps you make sure that the simulation is being delivered and counted at appropriate times.
The Challenging Part:
The more challenging part is the therapy piece of it, such as delivering the therapy as well as coordinating all the players within the health system. In terms of the players, you have the patient and their family, neurology, neurosurgery, and the therapist themselves.
From the patient and family standpoint, they come into this system after learning about the therapy, but they also must be willing to come to get the therapy three times a week which requires extensive scheduling and coordination. The patients also have the real concern of a procedure–any procedure does carry its risk.
From a neurology and neurosurgery standpoint, you want to make sure that these patients are ideal candidates for this intervention with medical and surgical screening.
Across all these players, you want to coordinate with scheduling and administration so the process is seamless.
For the actual therapy, you want to ensure that you are thinking about this therapy differently than how we traditionally think about therapy in chronic stroke at an outpatient level. At an outpatient level, we are mostly focusing on compensation, however with this approach, your focus is on remediation and making sure that there are high repetitions, challenging progressive, and high intensity tasks that are being performed to drive that that neuroplasticity.
Since the sessions are 90 minutes long, you must work with your admin personnel to be able to schedule this amount of time, as it is longer than a typical session. This much time is needed to be able to provide the intensity and level of repetitions required for this therapy to be effective. The other side of this is the patient tolerance piece–90 minutes is a long time. Oftentimes by this point in their progression and their state of stroke, they’re not moving their arm around, so then to go in and use their arm three times a week for 90 minutes at a time, you need to build up their tolerance and make sure that they are motivated to do this kind of an intensive program.
The therapy is key to successful patient outcomes. VNS is like a microphone– if you have no voice, a microphone is not going to do anything for you. You need to have something to start, and the therapy is that key piece that the VNS can amplify. The outcomes are only going to be as good as the therapy and the VNS is only going to work as good as the therapy is.
The Appropriate Candidates for Paired VNS Therapy:
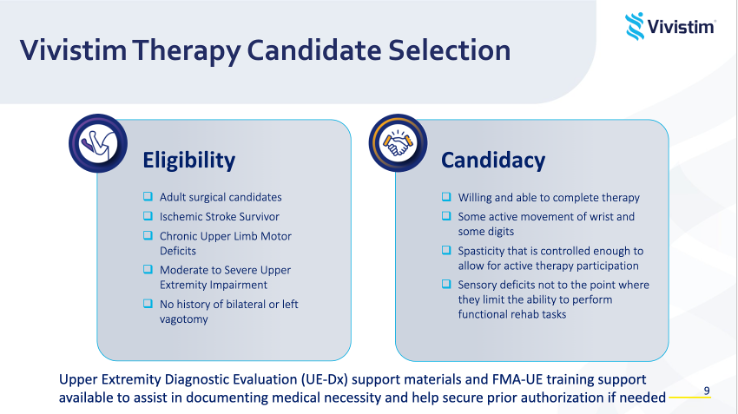
You need to ensure the patient is a good surgical candidate and that they can tolerate the procedure.
This intervention is approved for people with chronic ischemic stroke with moderate to severe upper extremity impairment. Patients need to have some active movement in their wrist and digits because if they do not have anything, the VNS is not going to have anything to build. If their arm is flaccid or so tight that they cannot participate well, this may not be the best therapy for them now. The other piece that we often tell patients is to time their Botox to when they are going to start therapy. If they can get their Botox at the start of therapy and loosen up a little, then the VNS will hopefully have better results.
Along with that, when you meet your patients, it is important to set their expectations. There are going to be people that have great recovery and outcomes but there will also be people who are not there yet but can benefit at a slower or longer pace. For some, it may take longer after the completion of those six weeks of in-clinic therapy, but they can continue to use their device at home and in home exercise programs to continue to make gains. The results of the long-term study follow-up show that people are making gains 3 years post-implantation, so there is a lot of promise immediately and in the future that they can progress in terms of function.
This is a very intense program, and you want patients who are consistent, motivated, willing, and able to complete the therapy. Not just from a fatigue standpoint, but also from a logistical standpoint that they can get to therapy three times a week and will not cancel their sessions.
How to Implement Paired VNS Therapy Sessions to Maximize Patient Outcomes:
The in-clinic portion of the therapy are 90-minute sessions, three times a week, for six weeks. The rehab is delivered by a PT or an OT and the therapist will trigger the VNS at key moments during a task, timing the stimulation and when you deliver the stimulation to what goals you are trying to address. For example, if you are working on grasp then you are going to stimulate at the moment that they are initiating that grasp pattern; if you are working on release, you are going to stimulate at the moment the patient is initiating the release. It is goal based, task-specific training, with high repetition yield.
Following those six weeks, patients go into a home-based mode–that means that the patient can trigger it via a magnet swipe, and it will turn on to give a continuous stimulation every 10 seconds for 30 minutes. The instructions are to pair it with a daily home exercise program that is deliberate and created in collaboration with the therapist and the patient.
Principles Underlying This Therapy:
These principles are the same as experience dependent plasticity and involve high repetition yield. Over 300 repetitions per session is the goal, with 30 to 50 repetitions of each type of movement or task.
Emphasizing mass practice but also thinking about variable practice. This helps with patient engagement, attention, and cognitive factors that are important in learning and motor learning.
You can use different objects to work on similar grasps as well as perform tasks in various positions: sitting, standing, dynamic standing, or walking. The sky is the limit with creativity in terms of how you are designing and developing these tasks in collaboration with your patient.
Active movement, task specificity, and salience are so important because this approach is all active movement on the patient’s part. There is little hand-over-hand assistance from the therapist, which forces the patient to perform these tasks on their own, using their more impaired arm. It also forces you as a therapist to be creative in how you are developing the tasks that are moving them towards their goals.
Salience is an important part of this puzzle because if it is motivating and engaging for the patient, it will enhance that neuroplasticity piece even more.
Pairing VNS with Rehab:
To watch the full webinar and see real video examples of Paired VNS with Rehab, click here.
If you would like to learn more about Vivistim’s unique Paired VNS Therapy and how it can help improve motor development after a stroke, contact us and we will connect you with a Vivistim representative. We also encourage you to explore the other pages of vivistim.com to find additional information and resources.
Additional Resources:
The MicroTransponder® Vivistim® Paired VNS™ System is intended to be used to stimulate the vagus nerve during rehabilitation therapy in order to reduce upper extremity motor deficits and improve motor function in chronic ischemic stroke patients with moderate to severe arm impairment. Do not use if you have had a bilateral or left cervical vagotomy. Risks may include, but are not limited to pain after surgery, hoarseness, bruising, swelling, coughing and throat irritation. Infection leading to explant is a risk associated with any device surgery. For full safety information, please see www.vivistim.com/safety. Individual results may vary.
©2024 MicroTransponder Inc. All rights reserved. Vivistim, Vivistim Therapy and Paired VNS are trademarks of MicroTransponder Inc.
25-0001-0047 Rev. 0